Widecillin
"Trusted 1000mg widecillin, antibiotic ointment for babies".
By: A. Nemrok, M.B. B.CH. B.A.O., M.B.B.Ch., Ph.D.
Professor, Southwestern Pennsylvania (school name TBD)
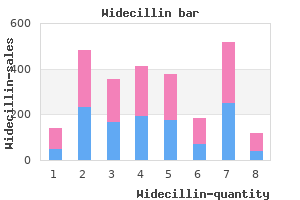
Depending on the depth of invasion antimicrobial wood sealer buy cheap widecillin 625mg line, these early lesions are treated with brachytherapy alone or brachytherapy combined with external beam irradiation antibiotic kidney stones cheap 625 mg widecillin amex, and cure rates exceed 95% infection wisdom tooth extraction buy cheap widecillin online. The goal of both treatments is to destroy malignant cells in the cervix antimicrobial door mats 625mg widecillin otc, paracervical tissues, and regional lymph nodes. Patients who are treated with radical hysterectomy whose tumors are found to have high-risk disease features may benefit from postoperative radiotherapy or chemoradiation. Because young women with small, clinically node-negative tumors tend to be favored candidates for surgery and because tumor diameter and nodal status are inconsistently described in published series, it is difficult to compare the results reported for patients treated with surgery and those treated with radiotherapy. In the surgery arm, findings of parametrial involvement, positive margins, deep stromal invasion, or positive nodes led to the use of postoperative pelvic irradiation in 54% of patients with tumors 4 cm in diameter and in 84% of patients with larger tumors. Patients in the radiotherapy arm received a relatively low median dose to point A of 76 Gy. With a median follow-up of 87 months, the 5-year actuarial disease-free survival rates for patients in the surgery and radiotherapy groups were 80% and 82%, respectively, for patients with tumors that were 4 cm, and 63% and 57%, respectively, for patients with larger tumors. The authors reported a significantly higher rate of complications in the patients treated with initial surgery, and they attributed this finding to the frequent use of combined-modality treatment in this group. For patients with similar tumors, the overall rate of major complications is similar with surgery and radiotherapy, although urinary tract complications tend to be more common after surgical treatment and bowel complications are more common after radiotherapy. Surgical treatment tends to be preferred for young women with small tumors because it permits preservation of ovarian function and may cause less vaginal shortening. Radiotherapy is often selected for older, postmenopausal women to avoid the morbidity of a major surgical procedure. Because patients with these risk factors have an increased rate of pelvic disease recurrence, surgical treatment is usually followed by postoperative irradiation or chemoradiation, increasing the overall length of treatment and side effects of treatment. Two prospective randomized trials43,296 demonstrated that patients who are treated with radiation for bulky stage I cancers benefit from concurrent administration of cisplatin-containing chemotherapy. A third study suggested that patients who require postoperative radiotherapy because of findings of lymph node metastasis or involved surgical margins also benefit from concurrent chemoradiation. This procedure involves en bloc removal of the uterus, cervix, and paracervical, parametrial, and paravaginal tissues to the pelvic sidewalls bilaterally, with removal of as much of the uterosacral ligaments as possible (see. The uterine vessels are ligated at their origin, and the proximal third of the vagina and the paracolpium are resected. Ovarian metastases are rare in the absence of metastases to lymph nodes or other sites. If intraoperative findings suggest a need for postoperative pelvic irradiation, the ovaries may be transposed out of the pelvis. Radical hysterectomy is increasingly being performed using a laparoscopic approach with or without robotic assistance. Preliminary results suggest that outcomes of laparoscopic radical hysterectomy are similar to those achieved with radical hysterectomy performed using the traditional abdominal approach. Intraoperative and immediate postoperative complications of radical abdominal hysterectomy include blood loss, ureterovaginal fistula (1% to 2% of patients), vesicovaginal fistula (<1%), pulmonary embolus (1% to 2%), small bowel obstruction (1% to 2%), and postoperative fever secondary to deep vein thrombosis, pulmonary infection, pelvic cellulitis, urinary tract infection, or wound infection (25% to 50%). Severe long-term bladder complications are infrequent and are related to the extent of the parametrial and paravaginal dissection but not to the type of surgical approach (abdominal or laparoscopic). Since then, it has been demonstrated that when these procedures are performed by experienced surgeons, the cure rates are high and many women are able to carry subsequent pregnancies to viability. However, patients who had radical trachelectomy had more problems with dysmenorrhea, irregular menstruation, and vaginal discharge; in addition, 14% had cervical suture problems, 10% had isthmic stenosis, and 7% had prolonged amenorrhea. Patients with extensive endocervical extension are poor candidates for fertility-sparing surgery. Initial results of this trial, published in 2000, demonstrated significantly improved rates of pelvic disease control and survival for patients who received chemotherapy (Table 72. Although outcomes are poorer for patients with larger tumors, even these are frequently curable with a combination of external beam irradiation and brachytherapy. Patients are usually treated with a combination of external beam irradiation to the pelvis and brachytherapy. Even relatively small tumors that involve multiple quadrants of the cervix are usually treated with total doses of 80 to 85 Gy to point A. Although patients with small tumors may be treated with somewhat smaller fields than patients with more advanced locoregional disease, care must still be taken to adequately cover the obturator, external iliac, low common iliac, and presacral nodes. Patients with involvement of the pelvic lymph nodes, parametria, or surgical margins were excluded. Patients who received adjuvant radiotherapy experienced a 46% reduction in the risk of recurrence (p = 0.
At the four-chamber view plane flagyl antibiotic for sinus infection order 375mg widecillin amex, the right and left lungs are seen and the rib cage assessed antibiotic vs antibacterial widecillin 625 mg overnight delivery. Comprehensive evaluation of the lungs in axial views requires the assessment at the level of the four-chamber view antibiotics for dogs lyme disease buy widecillin online pills. B: Axial view of the thorax at the level of the four-chamber view in the same fetus virus protection for iphone purchase widecillin no prescription. Comprehensive evaluation of the fetal lungs in axial views requires an evaluation at the level of the four-chamber view (A) and the threevessel-trachea view (B). The cardiac axis and position as evaluated in the four-chamber plane (A) is not only important for detecting cardiac abnormalities, but also for suspecting lung anomalies. The ribs can also be assessed from an axial plane of the chest at the level of the four-chamber view. In our opinion, the evaluation of the diaphragm is best achieved in coronal views. In these planes the diaphragm muscle and tendon on the right and left chest can be well visualized. The transvaginal approach improves visualization of all chest structures due to higher resolution. Clear visualization of the lungs can be achieved from about the 12th week of gestation onward. Note in the right thorax (A) the slightly hyperechoic lung as compared to the liver and the diaphragm in between. The parasagittal view on the left (B) shows the lung, portion of the heart, the diaphragm, and the stomach (asterisk). B: An axial plane of the chest at the level of the four-chamber view in the same fetus demonstrating the ribs laterally. The volume displays the coronal planes of the fetus showing in the chest the thoracic cage with ribs (yellow arrows), lungs, heart, diaphragm, and in the abdomen the stomach (asterisk), liver, and bowel. Hydrothorax may occur unilaterally or bilaterally and may be primary or secondary. Primary hydrothorax is a diagnosis made after excluding causes of hydrothorax, which are many, and involve fetal lung or cardiovascular malformations, fetal arrhythmias, infections, chromosomal aneuploidy, and others. In a prospective study between 7 and 10 weeks of gestation, hydrothorax was found in 1. Follow-up of 14 fetuses with bilateral hydrothorax diagnosed in the first trimester showed only one survivor. A high incidence of chromosomal aneuploidy, including monosomy X, was also reported. Ultrasound Findings Accumulation of fluid around the lungs is relatively easy to detect on ultrasound on axial. A typical sign for hydrothorax involves the presence of fluid between the lateral borders of the lungs and the ribs. This sign allows for differentiating hydrothorax from pericardial effusion, which can be difficult in some cases. In pericardial effusion, the fluid surrounds the heart and is on the medial aspects of the lungs. The presence of severe hydrothorax results in lung compression with the typical "butterfly" appearance of the lungs. Diagnostic or therapeutic thoracocentesis is typically reserved for the second or third trimester of pregnancy. Associated Abnormalities Associated abnormalities are many and include cardiovascular and skeletal malformations, fetal arrhythmias, chromosomal abnormalities including monosomy X, trisomy 21, Noonan syndrome, and hematologic conditions. Persistence of hydrothorax is later associated with pulmonary hypoplasia due to compression of lungs. Increased pressure in the thoracic cavity, associated with bilateral hydrothorax, may lead in the second trimester to reduction in venous return to the heart, resulting in fetal hydrops and polyhydramnios due to compression of the esophagus. The diaphragmatic defect is most commonly located in the posterolateral part of the diaphragm (Bochdalek type). Other types of diaphragmatic defects include the parasternal region of the diaphragm (Morgagni type) located in the anterior portion of the diaphragm, the central tendinous region of the diaphragm located in the central septum transversum region of the diaphragm, and hiatal hernias occurring through a defective esophageal orifice. It is reasonable to assume however that the timing of herniation of intraabdominal content into the chest can be delayed to the second trimester or beyond, as it is dependent upon the size of the diaphragmatic defect and intraabdominal pressure. This effusion spontaneously resolved on follow-up ultrasound in the second trimester of pregnancy.
Radiologic imaging represents the bulk of diagnostic studies for aggressive bone conditions infection 86 purchase genuine widecillin on-line. Plain roentgenograms include orthogonal views of the primary skeletal site and two views of chest as an initial assessment of metastatic pulmonary disease treatment for recurrent uti by e.coli order 1000mg widecillin. A bone scan aids in determination of primary site activity antibiotics for acne bacteria discount widecillin 375mg on-line, and the presence or absence of polyostotic or metastatic disease antibiotics for dogs with heartworms order cheap widecillin line. In the case of suspected primary bone malignancy, supreme caution must be taken with respect to the manner in which the biopsy is undertaken. Excisional (resection) biopsy can be considered for smaller lesions that can be completely excised with negative margins and without undue functional compromise; an atypical or low-grade chondrosarcoma arising in an osteochondroma is an example of this type of biopsy procedure. Whenever an open biopsy procedure is chosen, careful attention must be paid to incisional length (short) and placement (in line with the definitive resection procedure), dissection planes (through rather than between muscular planes), and avoidance of neurovascular exposure, bleeding, and infection. The risk of diagnostic errors and complications increases by as much as 12-fold when the biopsy is improperly done. While local control measures (surgery and/or radiotherapy) are critical to the treatment of patients with Ewing sarcoma, systemic therapy is equally critical to attaining cure. These results definitively established the importance of doxorubicin in the management of Ewing sarcoma, but also demonstrated that whole lung radiation may prevent some cases of relapse even in the absence of documented lung metastasis. In addition, they identified large tumor size and poor histologic necrosis to neoadjuvant chemotherapy as potential adverse prognostic factors in this setting. Nevertheless, these results suggested that more frequent chemotherapy cycles were beneficial and/or that more protracted cyclophosphamide exposure was beneficial. In the intensive schedule, patients received higher doses of doxorubicin and cyclophosphamide given in cycles administered every 3 weeks. In the protracted schedule, patients received lower doses of these agents and exposure of the cyclophosphamide was distributed across 6 sequential weeks. This design resulted in significantly greater early doxorubicin exposure in the intensive arm as well as a slightly higher cumulative doxorubicin exposure in that arm. Among 214 eligible patients, all outcome measures (relapse-free, disease-free, and overall survival) were superior for patients randomized to the intensive arm. The French cooperative group conducted a nonrandomized trial in which ifosfamide replaced cyclophosphamide throughout neoadjuvant and adjuvant chemotherapy that also contained vincristine, doxorubicin, and dactinomycin. Replacing cyclophosphamide with ifosfamide did not appear to improve outcomes compared to historic controls, suggesting that ifosfamide (without etoposide) is not active in this setting or that eliminating cyclophosphamide exposure altogether was deleterious. Compared to historic controls treated with cyclophosphamide, relapse-free and overall survival appeared more favorable with the use of ifosfamide. These results suggested that the use of ifosfamide helped to mitigate the adverse impact of large tumor size and/or axial tumor site. All patients received the same duration of therapy and the same cumulative dose of doxorubicin, with actinomycin-D substituted once patients received that cumulative doxorubicin dose. A total of 518 eligible patients were randomized, 398 of whom had localized disease at study entry. Patients in the experimental arm received higher doses of ifosfamide and cyclophosphamide during cycles of chemotherapy. All patients received approximately the same cumulative doses of chemotherapy such that patients on the experimental arm completed therapy earlier than patients on the standard arm. There was no statistically significant difference in event-free survival between the standard arm and the experimental arm, demonstrating that higher-dose therapy did not improve outcomes. Patients randomized to the interval-compressed arm had a significantly greater 5-year event-free survival (73% versus 65% for patients randomized to the standard arm). Of note, the role of interval compression in patients with newly diagnosed metastatic Ewing sarcoma has not been evaluated. These patients were then randomized to receive this same therapy in the adjuvant setting or this same therapy with cyclophosphamide substituting for ifosfamide. Among 155 randomized standard-risk patients, there was no difference in event-free or overall survival between patients who received ifosfamide or cyclophosphamide in the adjuvant setting. These results do not fully clarify the role of ifosfamide in this group as all patients received ifosfamide in the neoadjuvant setting. In particular, patients deemed high-risk due to large localized tumors appeared to benefit from the addition of etoposide, whereas patients with metastatic disease did not appear to benefit from etoposide. For both groups, participation in a cooperative group clinical trial should be strongly considered. The combination of topotecan with cyclophosphamide has shown activity in this population.
Syndromes
- Pain
- Bloody stools
- You have symptoms of narcolepsy
- Multiple myeloma
- Numbness
- Lymph node biopsy
- Pendunculated -- occurring on a long stalk on the outside of the uterus or inside the cavity of the uterus
One group has reported three cases of laparoscopic port-site recurrence; however drag virus purchase widecillin 1000 mg without prescription, in all three of these cases bacteria without cell wall purchase widecillin with a visa, the tumor was spilled from the operative specimen bundespolizei virus buy generic widecillin 1000mg online, allowing growth of the tumor tissue at the trocar sites virus 8 states order widecillin 1000mg otc. All limited resection endoscopic procedures require vigilant follow-up with an endoscopic reevaluation on a regular schedule because recurrence is quite common. The bladder here is open to reveal the distal ureter, which tunnels within the wall of the bladder. Because recurrences and urothelial atypia are usually distal in the ureter to the index lesion, it is reasonable to spare the kidney without undue risk of recurrent disease. Surgically, it is possible to remove approximately half of the distal ureter and reimplant it in the bladder. For upper ureteral tumors, replacement of the ureter with a segment of the ileum may be considered. Although segmental resection is becoming more accepted for mid and distal ureteral tumors, radical nephroureterectomy does remain the gold standard, especially for tumors in the proximal ureter and tumors with extensive ureteral involvement. N3 Results of Surgical Therapy the success rate of surgical procedures is primarily influenced by the pathologic stage of the disease at the resection (Table 65. Tumors lower in the urinary tract have a better prognosis when matched by stage with tumors higher in the ureter and pelvis. Prognostic factors, recurrence, and survival in transitional cell carcinoma of the upper urinary tract: a 30-year experience in 252 patients. Urology 1998;52:594601, with permission 5-year actuarial disease-specific survival rates by primary tumor pathologic stage were 100% for noninvasive tumors (Ta and Tis), 92% for pathologic stage T1, 73% for pathologic stage T2, and 41% for pathologic stage T3. The type of open surgical procedure used (nephroureterectomy in 77% of the patients compared with a kidney-sparing approach used in 17%) was evaluated by a univariate and multivariate analysis. Patients undergoing nephroureterectomy were found to have a significantly improved recurrence-free and disease-specific survival on multivariate analysis but not on the univariate analysis. However, as discussed previously, in other more recent series, patients with ureteral cancers who were appropriately selected for kidney-sparing resections did not have a poorer outcome. Adjuvant Topical Therapy Following Local Excision Only In cases in which endoscopic resection is performed, topical immunotherapy or topical chemotherapy may be important in preventing or delaying local tumor recurrence. Brookland and Richter267 have reported localregional recurrence in 45% and 62%, respectively. Most series report a close association between local failure and distant metastasis, although whether the association is causal or simply synchronous cannot be determined from the small numbers in the series. Radiation has been employed as an adjuvant therapy with mixed results reported in the literature (Table 65. Another study showed no advantage to radiation, but the radiation doses given were inadequate. Therefore, it is difficult to determine the true benefit of adjuvant radiation, if any. The small size of these two series and the biases inherent in this kind of retrospective review make it difficult to draw conclusions. Very little published data exist to guide physicians managing patients with a local relapse following a nephroureterectomy. If the relapse is bulky and metastases are present elsewhere, then palliation with chemotherapy would be the most appropriate course. When the relapse appears isolated and the patient relatively vigorous, consideration can be given to an aggressive approach that holds out the chance for cure. The first step would be to downsize and perhaps improve the respectability of the recurrence using external radiation to a modest preoperative dose of 30 to 45 Gy along with sensitizing chemotherapy. An attempt could then be made at resection or debulking and, if the facility were available, intraoperative radiation could then be given directly onto the tumor bed or onto an unresectable mass, with the bowel and other critical organs displaced out of the field. Such an approach allows for the delivery of high doses of radiation to the target without the risk of bowel injury that is present when managing such disease using external radiation treatment alone. Adjuvant Combined-Modality Therapy: Advanced Primary Tumors the most appropriate treatment for invasive transitional cell cancers of the upper urinary tract is nephroureterectomy. Despite aggressive surgery, cure rates are low when the disease has spread beyond the muscularis, with 5-year survival rates varying between zero and 34%.
Discount widecillin 625 mg line. safeguard antibacterial soap 1995 commercial.